If you lose your Medicaid coverage, you can take action to reinstate your coverage, or find another plan through the Marketplace. You could lose coverage for a few different reasons:
- Case 1: You lost your coverage due to procedural reasons (Ex: You didn’t complete the proper paperwork or the state Medicaid agency did not receive your eligibility documentation).
- Case 2: Your renewal application was incomplete or missed the renewal deadline.
- Case 3: You no longer qualify for Medicaid coverage. This can happen when your income changes or you have a change in your household size. You could also become disqualified if you received coverage under Medicaid expansion and now your income may be too high. If you qualified due to a temporary disability determination that ended, that can also make you ineligible.
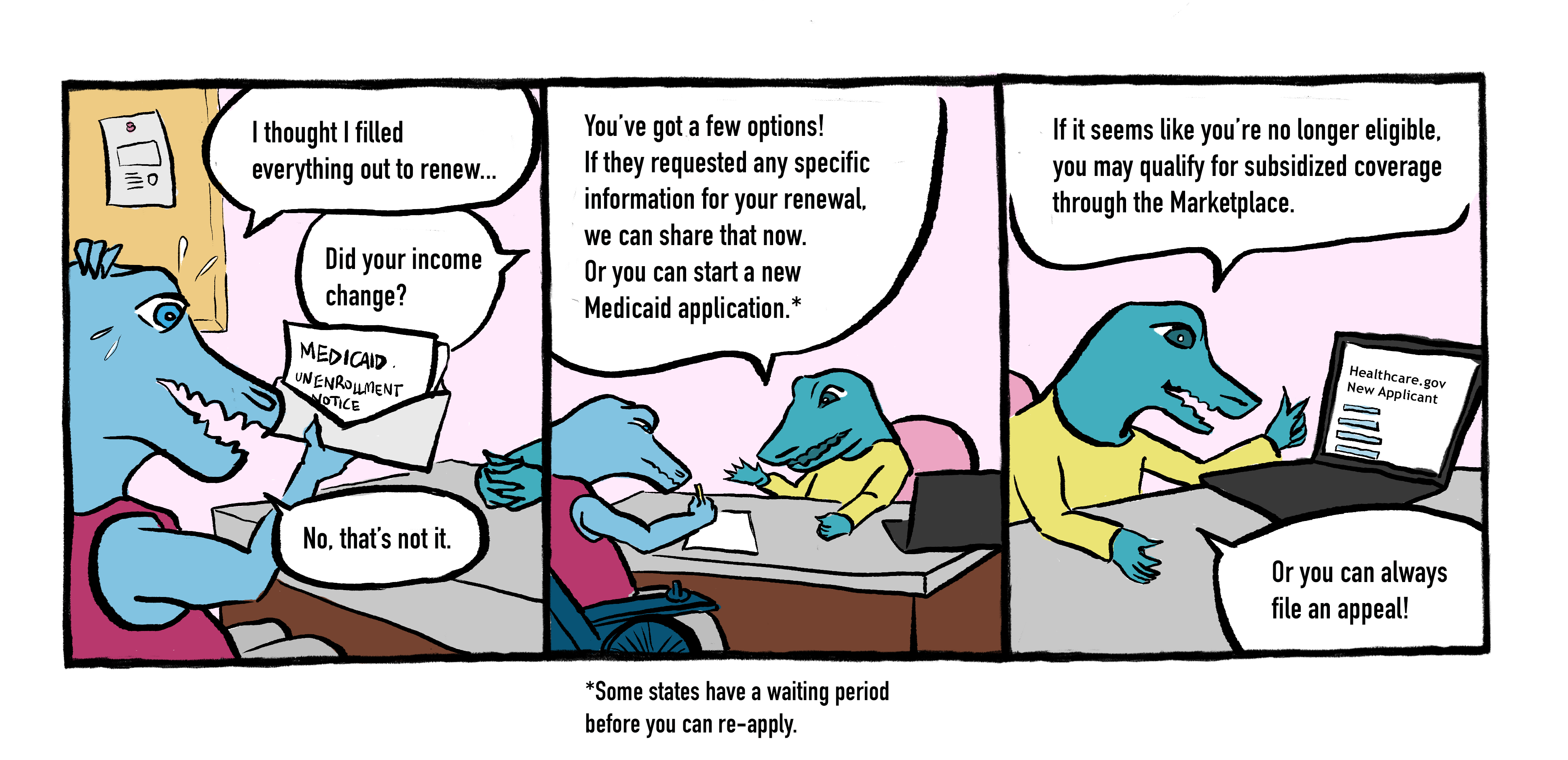
If you lose your Medicaid coverage, you have options:
- Complete your Redetermination: If you are still eligible, you may simply need to provide information to your state Medicaid agency to complete your redetermination application. This needs to be done within 90 days after your coverage was terminated.
- Re-apply for Medicaid: 90 days after your coverage is terminated, you can reapply for Medicaid by completing a new application. Enrollment is year-round.
- Apply for Marketplace Plan: If you no longer qualify for Medicaid, consider applying for free or low-cost healthcare through the ACA Marketplace at Healthcare.gov. Enhanced premium tax credits are available until 2025 that can significantly decrease the cost of your plan.
- File an Appeal: You can appeal your state Medicaid agency’s decision. Find more information about appeals at the Centers for Medicare and Medicaid Services.
Read our Factsheet #19 on the End of the Medicaid Continuous Coverage Requirement for more detailed guidance on why you may have lost coverage, and what to do to regain it.