HOW MANY HAVE LOST COVERAGE?
Throughout the summer, we are publishing the NDNRC Update on a biweekly basis.
The Kaiser Family Foundation continues to update their Medicaid Enrollment and Unwinding Tracker with the latest figures and data on monthly Medicaid enrollment, renewals, and disenrollments. As of June 14, 2023, almost 1.15 million Medicaid enrollees have lost coverage with 76% of all people being disenrolled due to procedural reasons, highlighting the importance of having the most up to date contact information and completing state renewal packets on time.
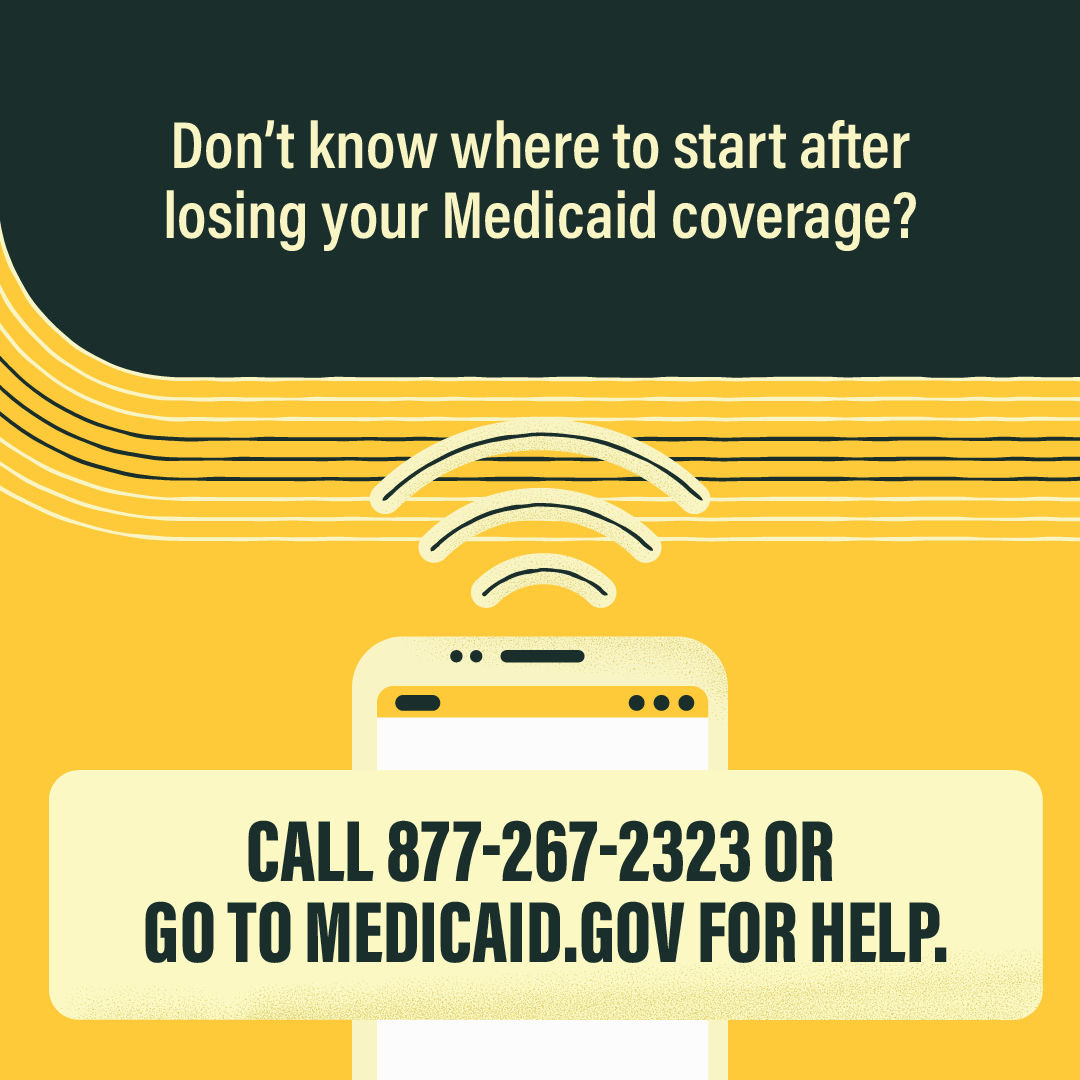
As part of our partnership with Community Catalyst, we have a project which highlights opportunities for people with disabilities to get access to health coverage through Medicaid or the ACA marketplace. As part of this project, they have graphics like the one below which highlight what people can do if they lose their coverage. These are available in the Community Catalyst Outreach Hub and on the Organizing for Outreach materials page.
CMS is trying to help states minimize the number of people who are losing their coverage. This week, they released new guidance to states on what they can do to provide flexibility to the number of children and families losing coverage as the redeterminations continue. To learn more, check out the CMS press release.
The Georgetown Center for Children and Families also released a blog post which examines this guidance from CMS and other steps which the agency is taking to help reduce the number of people losing coverage during the Medicaid unwinding.
As states continue to respond to the end of the COVID-19 public health emergency, the National Academy for State Health Policy has updated key resources for states and organizations to utilize. Blogs, briefings, and webinars based on telehealth and looking beyond the PHE are available on this site.
On Thursday, May 25, 2023, we hosted a webinar entitled “Medicaid Unwinding: What Advocates Need to Know.” That webinar has now been archived on our YouTube page with closed captioning.
Unwinding the Medicaid continuous coverage requirement has begun in many states, and in some states, people may have started losing their Medicaid eligibility. Over the last couple months we have been updating our “Medicaid Unwinding Resources” blog post which has links to various resources including our Medicaid unwinding flyer and recent additions like the Kaiser Tracker referenced above.
The Georgetown Center on Health Insurance Reforms has two new blog posts which look at pending legislation which would affect insurance coverage related to small employers and tele-health:
- A Wolf in Sheep’s Clothing: The Pitfalls of Treating Telehealth Coverage as an “Excepted Benefit”
- Proposed Expansion of Self-funding for Small Employers Would Roll Back Affordable Care Act Protections, Pre-empt State Insurance Oversight
The Kaiser Family Foundation released a brief on the current standards and proposed changes of the Medicaid managed care network. Current research findings suggest that MCO provider network directories can overstate Medicaid physician availability and adequacy standards, creating more access barriers to care. To solve these issues, states would need to monitor systems via an enrollee experience survey, submit an annual payment analysis, and enforce wait time standards.
The Department of Health and Human Services released a fact sheet this week which highlights new tools which are available for people with disabilities on ways to lower prescription drug costs through Medicare Part D.
Archives of our weekly updates are available on the NDNRC website.