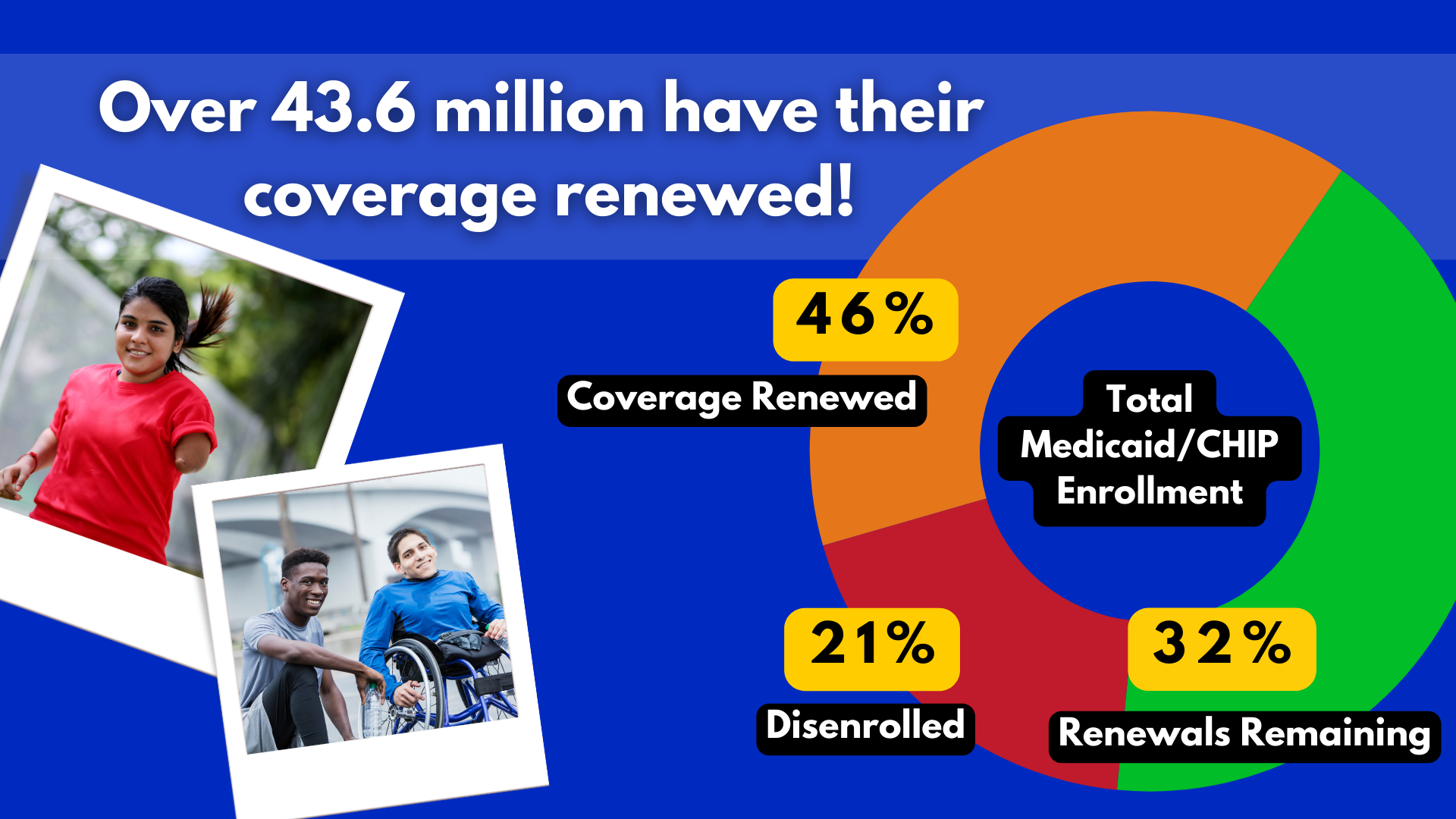
43.6 MILLION ENROLLEES QUALIFY FOR RENEWED COVERAGE
As of April 11, states have reported renewal outcomes for more than half of those enrolled in Medicaid/CHIP, according to data from the Kaiser Family Foundation (KFF) with 30.4 million renewals still remaining. 21% of those who completed the renewal process were disenrolled and 43.6 million enrollees were able to qualify for renewed coverage. The large range of disenrollment rates in each state varies, with the highest of 57% being in Utah and the lowest of 12% in Maine. Out of all states with available data, 69% of all those disenrolled were due to procedural reasons.
The Office of Inspector General (OIG) reported that the Centers for Medicare & Medicaid Services (CMS) did not ensure that selected states complied with Medicaid managed care mental health parity requirements. Georgetown University’s Center for Children and Families (CCF) covered this misstep where state deficiencies were reported.
Data on child health quality data has been made available through CCF’s State Data Hub. Here, information on how many children with Medicaid/CHIP coverage have gotten well-care visits, screenings, medications, and more, can be found.
The Commonwealth Fund (TCF) released a blog on using Medicaid to address youth populations’ mental health needs within school settings. 7 out 10 students in public schools reported seeking mental health services which have required schools to adopt better mental health programs.
TCF also reported on Medicaid eligibility and work requirements, as 67% of Medicaid enrollees were in school, working full-time, or even working part-time. Strict work requirements bar many potentially eligible enrollees from Medicaid coverage, like people with disabilities.
Archives of our weekly updates are available on the NDNRC website.