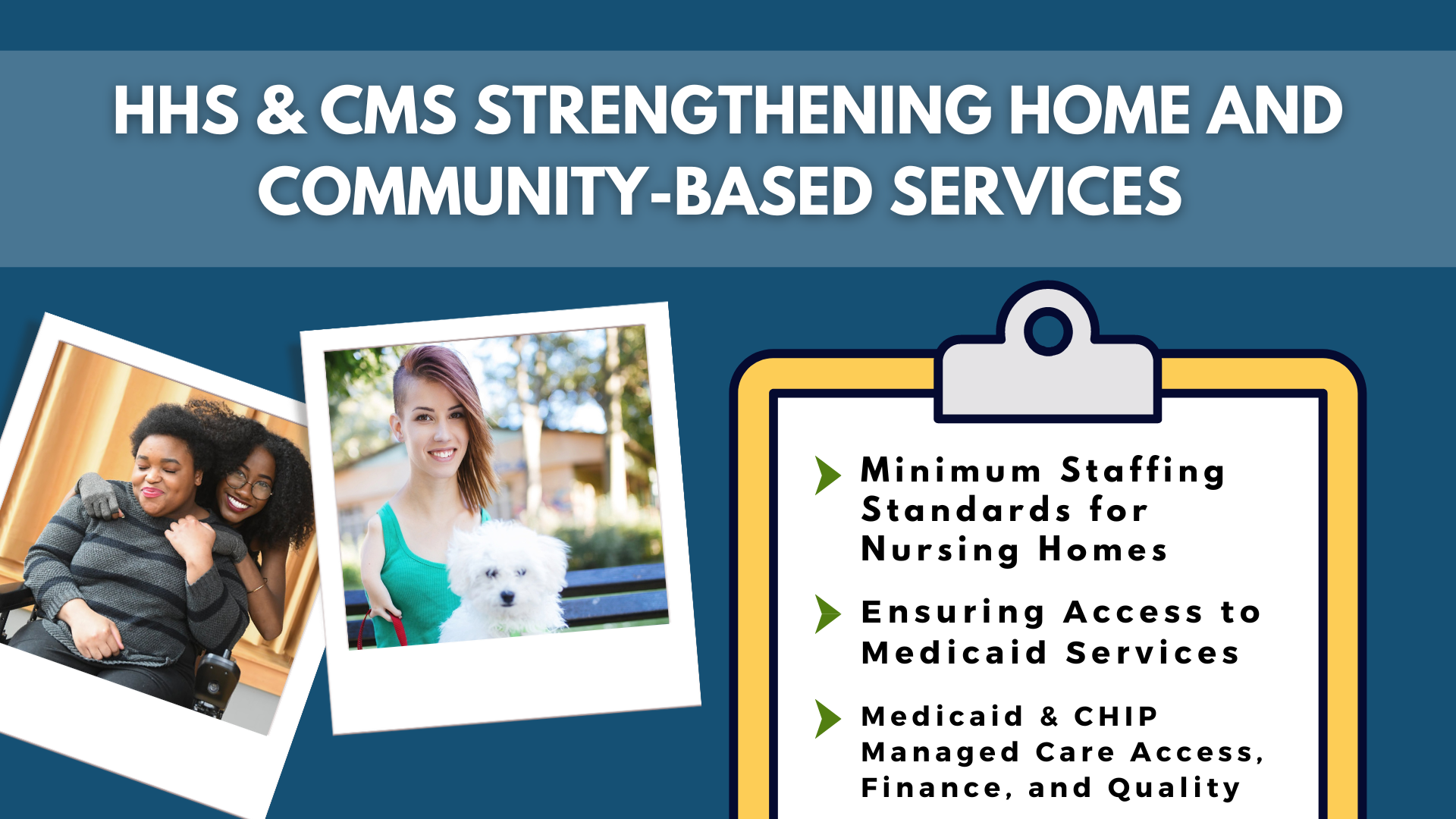
HHS AND CMS STRENGTHENING HCBS SERVICES
The Department of Health and Human Services (HHS) through the Centers for Medicare and Medicaid Services (CMS) have issued three final rules: minimum staffing standards for nursing homes, ensuring access to Medicaid services as an access rule that will strengthen home and community-based services (HCBS), and improving access to care for Medicaid and the Children’s Health Insurance Program (CHIP). This is great news for people with disabilities who utilize these services through CMS!
The Administration for Community Living also commented on this groundbreaking change issued by HHS and CMS, highlighting the fact that community living is a civil right that help make it possible for people with disabilities to live in their own homes, and connect and participate with their community.
The CHIRblog has continued to review the Final 2025 Payment Notice, specifically Marketplace standards and different insurance reforms. Relevant topics include new call standards, enhanced approval processes, and national standards for web brokers.
As of April 19, states have reported renewal outcomes for more than half of those enrolled in Medicaid/CHIP, according to data from the Kaiser Family Foundation (KFF) with 29.4 million renewals still remaining. 22% of those who completed the renewal process were disenrolled and 44.4 million enrollees were able to qualify for renewed coverage. The large range of disenrollment rates in each state varies, with the highest of 57% being in Utah and the lowest of 12% in Maine. Out of all states with available data, 69% of all those disenrolled were due to procedural reasons.
The National Health Law Program published COVID-19 continuous coverage and public health emergency unwinding resources. This list has materials retrieved from CMS, NHELP, and other federal agencies. Those who lost coverage during the unwinding of Medicaid should check out these resources to ensure access to continuous coverage!
KFF also covered recent guidance of Medicaid strengthening and expanding HCBS services alongside the Safter Communities Act of 2022. These provisions in tandem with new guidance from HHS and CMS will both help expand Medicaid partnerships in schools and the use of CHIP services to address behavioral health issues in school-aged children, an even more important provision for children with disabilities.
Review our latest factsheet on specific information on the availability of special enrollment periods, which are qualifying events that allow individuals to enroll in Affordable Care Act (ACA) Marketplace coverage outside of the open enrollment period, for people with disabilities and unique circumstances that they may face.
This factsheet is especially important, as the Centers for Medicare and Medicaid Services (CMS) has released new provisions due to the unwinding of Medicaid. See if you qualify for an ACA Marketplace plan at HealthCare.Gov and get covered today!
The CHIRblog covered the Administration’s finalization on limitations on junk health plans. This summary set new standards for short-term, limited duration health insurance and will be effective 75 days after being published in the federal register.
Georgetown University’s Center for Children and Families reported on new research that has linked postpartum Medicaid coverage to an increase in mental health care. This is especially important for mothers and children with disabilities in insuring the full spectrum of access to healthcare coverage and services.
Community might be one of the most important social factors that affects our health, shapes us, and gives our lives meaning. Who we connect with and rely on can play a huge role in our quality of life! Join the American Association on Health and Disability and register for our webinar on June 6th at 2:00 PM ET for a conversation on Community Care, Mental Health and the All of Us Research Program.
Archives of our weekly updates are available on the NDNRC website. Follow us on Twitter/X at @NDNRC!