MEDICAID RENEWALS AFTER THE PHE
Throughout the summer, we are publishing the NDNRC Update on a biweekly basis.
As the pandemic’s Public Health Emergency (PHE) eventually ends, states will start to reassess Medicaid and CHIP eligibility. This PHE saw almost a 20% increase in Medicaid and CHIP enrollment, a record 85 million people, according to Kaiser Family Foundation. However, only half of states have a plan for how they will advance renewal and eligibility when continuous enrollment coverage ends so the importance of Medicaid/CHIP users to renew coverage is more important than ever. Advocates should encourage Medicaid enrollees to make sure to update their contact information with most current mailing addresses, phone numbers, and email, as these are ways the state will contact them with a renewal form. CMS has set up a new webpage which provides guidance to Medicaid enrollees on what to do to make sure they are ready for the renewal process.
Last month our partners at the Center on Budget and Policy Priorities (CBPP) hosted a webinar which looked at special enrollment periods (SEPs). This webinar has now been archived for both the video recording and slides. Additionally, CBPP has updated its SEP charts which summarize what SEPs are available to various consumers.
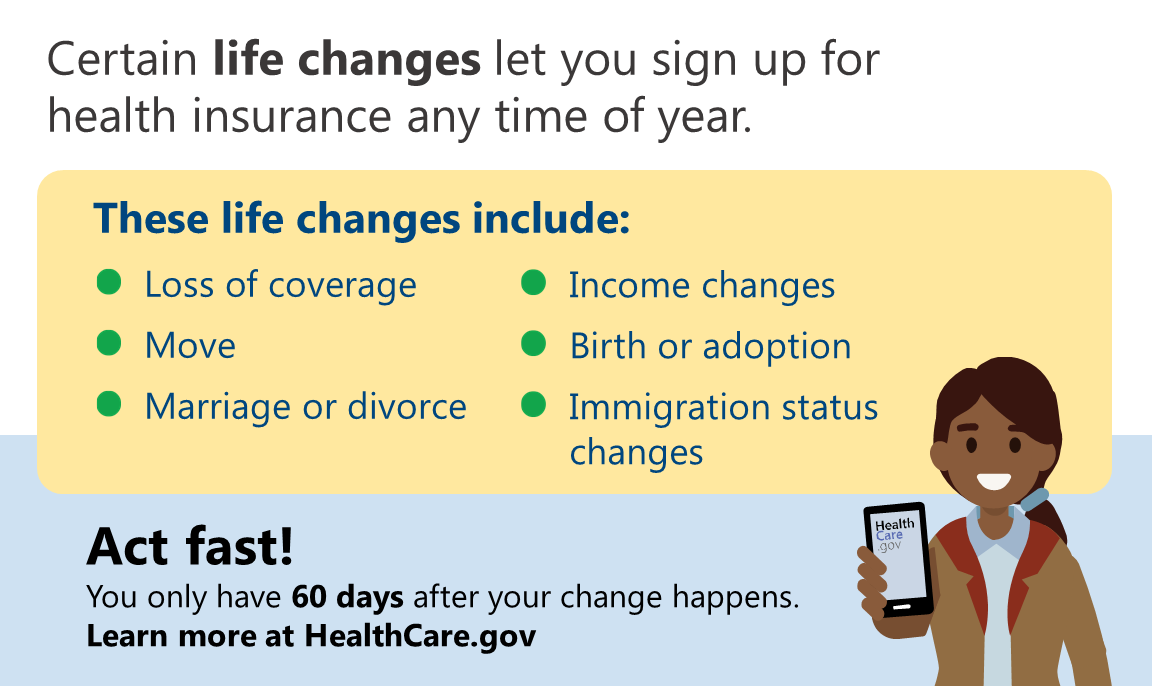
As part of our partnership with Community Catalyst, we have a project which highlights opportunities for people with disabilities to get access to health coverage through Medicaid or the ACA marketplace. As part of this project, we have resources like the image below which highlight the availability of special enrollment periods for certain life events. These graphics are available in the Community Catalyst Outreach Hub.
In case you missed it, we recently summarized all of the interviews we did as part of our Facebook live series on Get the Most Out of Your Coverage (GMOYC) for people with disabilities. The GMOYC interviews shed light on the positive impact that access to health insurance has, as well as tips on how to best use coverage. The summary of these interviews is available on both our AAHD website and our NDNRC website. You can also check out these full interviews on both our Facebook page and YouTube channel.
The American Rescue Plan Act (ARPA) did a lot to reduce premiums for marketplace consumers which led to record enrollment on the ACA marketplace. However, those enhanced marketplace subsidies are set to expire at the end of 2022. If you want to read more about the expiring enhanced premium tax credits which were part of ARPA and what Congress can do, here are some resources:
- Families USA: Unless Congress Acts, Health Care Costs Will Soon Skyrocket for People Who Buy Their Own Insurance
- Georgetown University Center on Health Insurance Reforms: Averting Premium Shock for Marketplace Consumers
- Kaiser Family Foundation: For ACA Enrollees, How Much Premiums Rise Next Year is Mostly up to Congress
- National Academy for State Health Policy: State-Based Marketplaces Say Many Will Lose Affordable Coverage if Premium Assistance Expires
This week marked the anniversary of the important Supreme Court decision of Olmstead v. L.C. which held that the ADA guarantees the right of people with disabilities to live in their community and receive supports and services. The Administration for Community Living published a blog post commemorating the anniversary of this important decision.
If you missed it in our last newsletter, the University of Kansas is once again conducting its National Survey on Health and Disability. To learn more about this survey, check out our news item.
Do you want to learn about the work we’re doing on the All of Us Research Program? Read more about it on our program initiative webpage.
Archives of our weekly updates are available on the NDNRC website.